As a new member of the Vidyo team, I had the privilege of attending Vidyo’s inaugural Healthcare Summit in Nashville earlier this month. Having attended all of the keynote sessions and some of the breakout sessions, I was inspired by the passion and energy of our speakers and delegates. (If you haven’t already read Elana’s recap of the Summit, or visited our blog in a while, please do so now – we have a wealth of new content.)
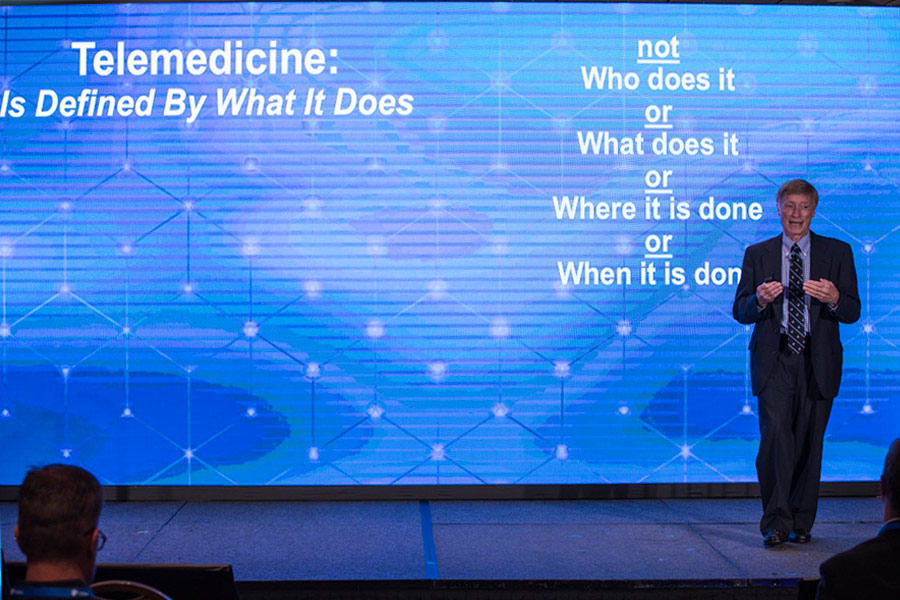
Dr. Jay Sanders delivers keynote: The Future of Healthcare
Perhaps the most profound revelation for me is that telehealth is simply healthcare (or telemedicine is simply medicine if you prefer). Many of our speakers made this simple but important point, including Dr. Jay Sanders, MD, founding member of the American Telemedicine Association, during his speech on the future of healthcare. The delivery mechanisms and tools to enable telehealth are varied, but the goals of telehealth programs are identical to the goals of healthcare: increase access to care and improve patient outcomes – efficiently and cost effectively.

Gilad Epstein, COO of OTN shares key ROI data from their telemedicine network
Based on what I learned from our speakers, I’ll go one step further and argue that telehealth initiatives, when implemented correctly, can massively accelerate achieving the core healthcare goals of any provider. Take the goal of increasing access to care, particularly in rural or disaster relief areas, a topic many of our speakers discussed.
- Gilad Epstein, COO at the Ontario Telemedicine Network (OTN), told us that as a result of OTN’s eConsult program, response time has been reduced to two days instead of weeks in specialties including dermatology, neurology, and cardiology.
- The Alaska Native Tribal Health Consortium (ANTHC) saves its patients, on average, 2.7 visits per year to its main Anchorage clinic. If you think about the simple fact that many Alaskan natives need to travel hundreds of miles to get to Anchorage, with a good number of these patients under palliative care, this is huge.
- Through Vidyo-enabled carts, Nemours Children’s Hospital provided disaster relief for victims of Hurricane Irma in 2017. Jeff Barnello, Senior Telehealth Technical Coordinator, perhaps said it best: “Never forget the vision. Every decision we make, we do it for the patients and families we serve.”
On the goal of improving patient outcomes, and doing so more efficiently and cost effectively, John F. “Fred” Thomas, PhD and Director of Telehealth at Children’s Hospital Colorado (CHC), painted one of the most compelling pictures. (Note that the scope of CHC’s telehealth initiative is truly staggering: 130-140 different telehealth interactions spread across 30 specialties, working across the care continuum – before admission, at the hospital, and after discharge.

Fred Thomas, PhD highlights key metrics that have delivered success in telemedicine programs across Children’s Hospital Colorado
Thomas took the audience through a real-world use case of the clinical utility of telehealth in pediatric mental-health emergencies. The traditional workflow looks something like this:
- The family calls 911
- The family and young patient wait 45 minutes for an ambulance, followed by a long drive to an urban hospital
- They wait another 4-20 hours in the ER before seeing a physician or mental health specialist
- More than half of patients are discharged without any care or treatment
According to Dr. Thomas, the traditional way is “traumatic for families and patients, especially ‘frequent fliers,’ very inefficient, and very expensive.”
Unlike the traditional workflow, CHC’s tele-behavioral health program enables trained mental health specialists to evaluate patients from a centralized yet distant location. The results?
- Reduced transfer rate by nearly 50%
- Improved patient satisfaction in regards to care – 98% of patients, parents, and providers were satisfied or extremely satisfied
- Dramatically reduced length of stay
- Decreased cost per encounter by $5,100 – from $8,600 to $3,500
Gilad Epstein of the OTN reinforced Thomas’s point about patient satisfaction with a very similar statistic from a different use case. At OTN, 97% of patients would recommend telehomecare. And on the issue of delivering care more cost effectively? OTN estimates that telehealth saves the Canadian healthcare system $77 million per year. Wow!
As I reflect on the Vidyo Healthcare Summit, reviewing my notes and writing this blog post, I’m grateful to be part of an organization that’s enabling our customers’ telehealth programs to succeed, and by extension, increasing access to healthcare and improving patient outcomes.
To be fair, not all is wine and roses in the telehealth world. I found it troubling that some of our customers are challenged by the issue of reimbursements and differences in parity laws among states. Much more is needed on this front, but it was great to learn that Nemours actually helped craft the language that led to telehealth legislation in New Jersey and Delaware, with Pennsylvania still in progress.
Healthcare providers in states that do not have telehealth parity should consider following a similar path. Get together with your legislators, colleagues, patients, and even competitors to push for parity. (More to come on the issue of reimbursements on our blog, so stay tuned!)
Based on all of the presentations and discussions I had at the summit, it became clear to me that telehealth is even more than just a natural extension of healthcare in a technology-driven world. The dozens of use cases that I observed led me to the conclusion that when done well, telehealth can be a massive accelerator that drives dramatic improvements in healthcare as a whole. Michael Hascker, Manager of Telehealth Technologies at the Medical University of South Carolina (MUSC), said it best during a Summit panel: “It’s our job to remove the ‘tele’ from ‘telehealth.’ It must become a fully integrated part of existing patient care and doing business.”
Recent Comments