
Introduction to the unconference session with Nick Adkins
As a new Vidyan I found our inaugural Vidyo Healthcare Summit to be a wonderful opportunity to immerse myself in the world in which our customers live and the issues with which they grapple daily. It was fantastic to learn about the beginnings of telemedicine and predictions about its future.
Our customers described their successes in telemedicine: reducing costs for their facilities and local governments, improving patient outcomes, and providing greater access to healthcare. All of these are very topical in public policy discussions at the moment. The experience validated my decision to join a dynamic business that enriches people’s lives by making real-time video communications ubiquitous.
Having been heavily involved in all the event planning, I had already seen all the presentations and had discussions with our speakers well in advance of the event. The real eye-opener for me was our unconference.
In this unfamiliar environment our audience, clinical practitioners, healthcare facility administrators, technologists, and other technology vendors, gathered together to generate and discuss topics about which they wanted to learn from their peers. With a very uncertain outcome!
Our facilitator, Joshua Kauffman, teased out a series of topics for all to discuss. Our commitment was to select from that list three topics of specific personal interest and to participate in smaller group discussions about those topics, at the end reporting back to the broader group.
The topics of most interest to me were: The Ethics of Data Usage and Redefining Normal. These sessions relate to individual patient data, how that data is stored, and how it’s made accessible to us as patients.
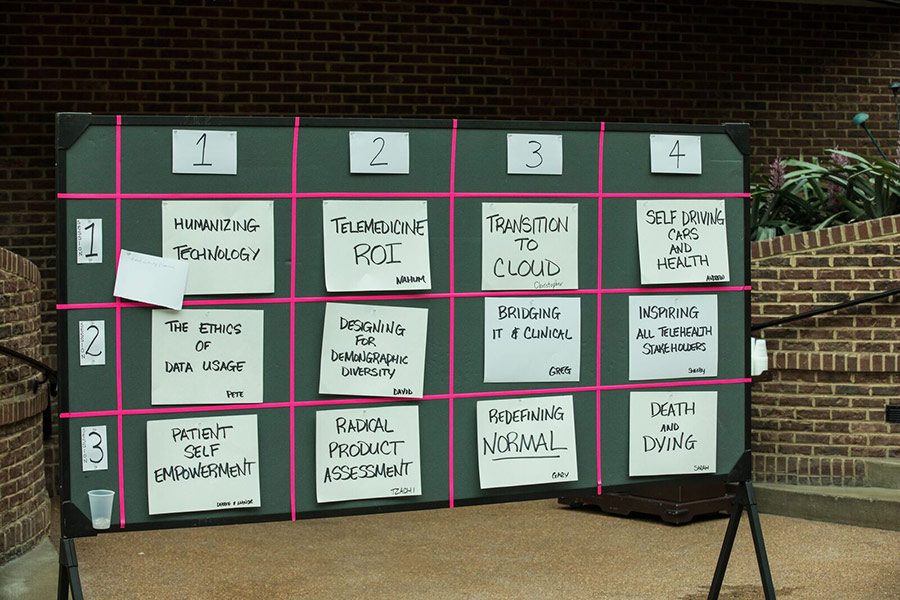
Unconference group discussion topics
The question of control was the main topic of focus in the the ethics of data usage discussion. Here the conversation revolved around ownership of data. The general feeling among the group is that we as patients should own our own data. There is a need for a system in which we can provide access to our data to whom we want and when we want.
This topic held a real resonance for me. I spent 14 years in the United Kingdom, where all records are stored centrally in the NHS system. Even when I moved to different counties and saw different GPs, every care provider had access to my records. Even those at a hospital emergency room could see my medical history.
Since returning to the US I’ve had several different insurers, as well as seen different doctors in New Jersey, where I currently live. No one has access to all my records, and only those who are affiliated with multiple facilities where I’ve been seen have access to records stored at those facilities. As a result, I have a long medical history that is not easily accessible to my current physician. It’s difficult for my physicians and other care providers to have a longitudinal record of my health.
That issue neatly intersected with the final session that I attended, Redefining Normal. This topic was broached by Dr. Jay Sanders, one of the summit’s keynote speakers, who spoke about the need for patients to be empowered and take ownership in determining their own healthcare. Dr. Sanders described a situation in which a family member may have regular blood pressure checks. Starting at a reading of 90 over 65, and over the years, running to a reading of 120 over 80, the family member would be told regularly, “that’s great, you’re normal.”
Of course, an increase of blood pressure as described really means that the patient is gradually becoming hypertensive over a period of several years. When her reading finally breaks the pane of glass described as normal, and the patient is told she’s ill, the reality is that she had been becoming unwell for quite some time. Earlier treatment could have made a world of difference.
So normal is a term that ought to be ascribed to us as individuals, not to us as an aggregate population. This is where the ownership of our data and the continuity of our medical records intersect with our personal health trends. How can my doctor in New Jersey know what’s normal for me when she’s missing 14 years of my history, data which resides in the United Kingdom’s NHS record?

Unconference members discuss the challenges of telehealth
One of the members of our group noted that our patient record is not merely a record of measurements. It’s also a record of observations by practitioners. He reminded us that we need to be careful to review those observations. In some cases it’s possible for notes to be written when we’re unconscious, not able to question them. In other cases those notes, sometimes casually written, can have unintended consequences, including affecting insurance costs.
The example given was a throwaway response to a question about smoking. When asked if he were a smoker, the person replied no, but that he’d smoked a cigar at New Years. Months later, when reading his own report, he saw that the doctor has annotated that he was a “part-time smoker.” This designation impacts his ability to purchase life insurance, as well as the cost. Having caught this, he ensured the note was expunged from his record. Not all of us are so fortunate!
Ideally what I want as a healthcare patient is ownership of my data. I want to be treated as if I were the owner of my data. I want access to it when I want it, and I want my healthcare providers to have access to it when I want them to have that access. And only when I want them to have that access. I want control over what’s written into my record.
Like Veruca Salt of Willy Wonka fame, I want it and I want it now!

Vidyo’s Vice President of Corporate Marketing, Gary Schwartz shares impressions from the unconference sessions
My takeaway from the unconference was to obtain my personal data records from the NHS. It will be fun trying to capture those. In the next few months I’ll recount my experience and let you know how well and to what extent I succeed in that endeavor. Look out for it.
And look out for more blogs and other content derived from our Summit. If you weren’t there, well, you won’t want to miss this next year!
Recent Comments