
Making Telehealth Work for You – Defining Your Strategy
Learn how to develop a successful virtual healthcare strategy, from identifying and overcoming common barriers to measuring its overall performance.

Learn how to develop a successful virtual healthcare strategy, from identifying and overcoming common barriers to measuring its overall performance.

For those considering a telehealth program, or thinking about adding to their existing one, the following guide is a comprehensive overview of how to get buy-in and support for a virtual health strategy.
These reflections from a pediatrician at a large practice are becoming more common in an industry that historically lags behind other markets in technology adoption. It is a positive indication of what lies ahead as healthcare gets more comfortable with using telehealth to advance patient outcomes. According to a recent telehealth adoption study commissioned by Vidyo, Inc., over 75% of nurses, physicians, healthcare administrators, and health IT professionals are currently using or plan to use telehealth solutions. That’s encouraging, given the advantages that live video, remote patient monitoring, and mobile health offer to both patients and providers.
FIGURE 1: VIRTUAL HEALTH ADOPTION IS ACCELERATING
Percentage of providers using virtual health in their organization or practice
Virtual Health adoption has grown by 33% over the period shown; however many are still reluctant to adopt.
Additional data from HIMSS Analytics shows that telemedicine use by providers has risen to 72%, having jumped from 54% in 2014. After consistently growing 3.5% annually, adoption has increased by roughly 9% since 2016. A study by global consulting firm Accenture found that virtual health could generate $10 billion in economic value annually across the U.S. health system, and experts point to virtual health as one of the most efficient and effective means of confronting social determinants of health obstacles because it breaks down barriers to accessing physical care.
Still, many stakeholders are reluctant to go too far down the virtual health path. Some cite cost or low demand as reasons. Others are uncertain about the regulatory and compliance environment for telehealth. But just as the stethoscope was initially greeted with some skepticism for its effectiveness as a diagnostic tool — only to be universally adopted and still in use 200 years later — virtual health is a solution whose time has come.
While commonly referred to as telehealth, a better term is virtual health because it is more descriptive. The prefix tele- implies something coming from a distance, when in fact the technology behind this term actually brings patient and provider closer together. Commenting on how virtual health is becoming a standard of care, Michael Haschker, Manager, Network Systems and Telehealth Technologies of the Medical University of South Carolina, says, “I see the ‘tele’ being removed from telemedicine and telemedicine as we know it today… (it is becoming) a part of the integrated healthcare system and health plans for people.”
Virtual health, as defined by Harvard Business Review, is the use of “enabling technology … to deliver health services in a way that is independent of time or location.” Through video visits, virtual rounds, and video responses to nurse calls, or by bringing specialist expertise to wherever it’s needed, virtual health is personalized healthcare without borders.

Just as a physician begins every consult with open-ended questions to discern the reason for a patient’s visit, the road to a virtual health strategy begins with a purposeful look at the benefits of adding or expanding virtual health in an organization. Does the physician practice want to treat more patients? Is the clinic trying to save money and improve access to care? It’s important to assess the challenges faced by the physician or health system to determine how virtual health would be beneficial.
To recruit other hospitals and health systems to join the Center for Telehealth at Dartmouth-Hitchcock Medical Center, Dr. Sara Pletcher listened carefully to the problems each organization was facing before advancing a particular solution. Not surprisingly, there was a lot of variation. From increasing regional market share to delivering on a set of patient-centered care metrics, virtual health adoption began with a strategic look at the problems it might be able to solve, followed by working to customize a successful solution.
Despite an awareness of the specific benefits telehealth can provide, the most enthusiastic telehealth adopter can be stymied by a number of barriers. According to the Vidyo study (see graphic on the following page), the primary reasons why providers are wary of adopting virtual health are:
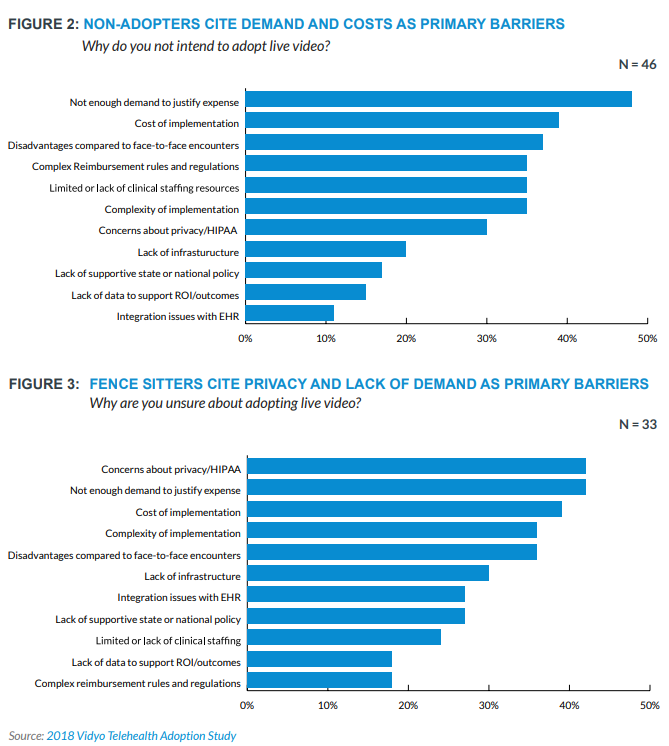
Without provider/clinician support, patient interest, or local market competition, demand for virtual health will seem low or nonexistent. In each of these instances, providers may be unclear about what exactly virtual health is and how it can help them simplify as well as expand their practice. In addition, providers often assume that patients prefer face-to-face treatment, when in fact many patients prefer the convenience and personal attention of a virtual visit. According to longtime telehealth advocate, Lauren Faison, from Tallahassee Memorial Healthcare: “Virtual care is here to stay. It’s not a fad. It is becoming much more commonplace and people will expect it from their physicians.”
Just as explaining the benefits of a particular drug or therapy to a patient is good medicine, clearly communicating the how and why of a virtual health program — to physicians and clinicians as well as to patients — is critical to getting stakeholders to truly understand the demand level for virtual health. It’s important to identify clinical champions in every use case, such as a physician on the provider side and a nurse/practice manager on the patient side who can advance understanding and buy-in for the rest of the team.
Poor experiences with EHR implementations that were expensive, complicated and took a great deal of time and IT resources have created lasting hesitancy for many in healthcare. It’s a rational fear for hospital systems overburdened with system implementation and update demands — just look at the recent earnings from Vanderbilt University Medical Center. The $3 billion medical system ended the first nine months of fiscal year 2018 with operating income of $44.4 million, down 60% from $110 million in 2017. Vanderbilt attributes the bulk of the income loss to the cost of implementing a new EHR
system.
While the Vanderbilt experience may be typical of EHR implementations, virtual health implementation is far less difficult because it can — and should — be done in a customized manner. Cloud-based virtual health platforms use fewer internal resources because they don’t require hardware and software management. For those reluctant to fully embrace moving to the cloud, hybrid models can be constructed that allow local traffic to stay local while also taking advantage of the convenience of cloud-based connectivity and management.
A recent Advisory Board update points to perhaps the biggest barrier to virtual health adoption: how providers will be paid. Recent legislation indicates that more favorable virtual health reimbursement models are emerging to swiftly lower this obstacle. Until recently, the Center for Medicare and Medicaid Services (CMS) reimbursed only for live audio-visual virtual health visits in rural areas. Despite these reimbursement barriers, Medicare volumes continue to grow. Early in 2018, CMS added remote monitoring services to the mix. Telehealth is now also a basic benefit of Medicare Advantage, rather than an optional add-on — all of these adjustments should fuel further Medicare telehealth volume.
FIGURE 4: Medicare policy changes are driving growth
MEDICARE FEE FOR SERVICE CLAIM VOLUMES CONTINUE TO GROW
On the commercial side, according to the Advisory Board, “There’s been a recent uptick in commercial parity legislation, which requires health plans to cover virtual services the same way they would cover in-person services. As of January 2018, 36 states and the District of Columbia have one of these laws in place — an increase of four states over the last year.” To stay abreast of state-by-state changes in virtual health reimbursement, the Center for Connected Health Policy website or the Advisory Board Primer are valuable resources.
Now that healthcare has earned the dubious distinction of being the industry most vulnerable to data breaches, it’s understandable that hospitals and health systems have a number of data privacy and HIPAA compliance concerns with virtual health. According to the HIMSS Analytics study, it’s an especially “great hurdle” for outpatient services. For those using virtual health for behavioral health purposes, there’s the added concern that household members could overhear private conversations between provider and patient.
To alleviate data privacy concerns, providers should be careful about the kind of virtual health solution in use. Asynchronous or store-and-forward telemedicine platforms are now showing up in primary care programs. Proponents say it gives them a better chance to use evidence-based care delivery practices at lower risk. However, video-exclusive platforms are generally more secure because they don’t store patient health information. Behavioral health uses can be improved by obtaining patient consent to have family participate.
No matter what the use case is, virtual consent forms should be in place between patient and provider, and any virtual health solution should include a business associate agreement (BAA) to ensure both contractual and regulatory compliance between vendor and provider.
Lack of clinical staff, integrations with EHR, and other infrastructure issues are important considerations for every health organization considering virtual health. Those who have successfully addressed them point to several factors for smooth adoption and integration:

With barriers reviewed and a list of desired benefits in hand, it’s time to get to work on an implementation strategy. Most hospitals and health systems will quickly discover that virtual health is not a one-size-fits-all solution.
As Dartmouth-Hitchcock’s Pletcher says, “Everyone has a favorite cookie. You can’t tell a Thin Mint guy all about the merits of a Tagalong and expect him to write something down on the order form.” The HIMSS Analytics study echoes the need for customization: “A telemedicine platform or use case is not universally valuable to all healthcare orgs/facilities.” Working through the specific virtual health benefits to your organization and openly discussing the hurdles to adoption are vital for successful adoption.
With strategy in hand, it’s time to execute. As with the adoption of any new technology, it’s not going to be smooth sailing. It’s wise to prepare in advance for the inevitable upgrades and software tweaks.
To measure performance and return on investment (ROI), make sure you have the right accountability procedures in place and work with your vendor to provide best practice recommendations on key performance indicator (KPI) dashboards. In addition to clinical measurements, patient feedback mechanisms and a formal patient communications strategy are vital KPIs to maintain.
If you’re unsure if the ROI estimates are a stretch but achievable, there are tools in the market to develop specific ROI, as well as third-party data for additional validation such as the analytics offered by Ignis Health and other HIT vendors.
Virtual health holds great promise for addressing a number of gaps in our health system, from the chronic shortage of primary care doctors to care for vulnerable populations in remote, hard-to-reach areas. Just as René Laënnec’s stethoscope revolutionized the practice of medicine, virtual health will transform the healthcare landscape for years to come.

Learn how to overcome disasters with continual video communications for planning and recovery strategies that save lives.
Learn how to enhance patient engagement with high-quality, real-time video for effective home care, improved outcomes, and reduced costs.
Recent Comments